While topographies are not necessary for the initial orthokeratology lens selection, they are critical for the ongoing success of treatment. Frequently, practitioners uncover valuable information that can improve patient outcomes and reduce lens remakes (as well as chair time). Analyzing the detailed topographical information at the onset of treatment can ensure the highest chance of a successful outcome.
What are the most important reasons for performing corneal topography?
Rule out corneal disease and unstable tear film
Ortho-K is contraindicated in patients with corneal ectasias such as keratoconus. It is important to rule out early signs of ectasia before proceeding, as the cornea may be difficult to assess once corneal reshaping has occurred.
In addition to astigmatism, progressive myopia is commonly seen in the early stages of keratoconus.1 The latest keratoconus prevalence studies suggest higher numbers than previously believed. This increasing prevalence is often directly attributed to earlier detection from improved imaging capabilities.2
By analyzing the quality of the topographical mires, practitioners often gain valuable information about the patients’ tear film stability. The tear film plays an important role in the hydrodynamic fluid force mechanisms of Ortho-K; practitioners should be cautious before proceeding in patients with moderate-severe ocular surface disease.
Determine complexity prior to starting treatment
It can be more difficult to achieve successful Ortho-K outcomes in patients with extremely flat or extremely steep keratometry measurements (K-values). Flatter than average K-values (41D or below) may limit the amount of myopic treatment possible, which can pose problems for higher myopes. Conversely, steeper than average K-values (48D or above) may be concerning regarding corneal ectasia. In cases where definitive ectasia is not evident on topography, practitioners should consider imaging of the posterior cornea (utilizing tomography instruments) to rule out sub-clinical corneal ectasia.
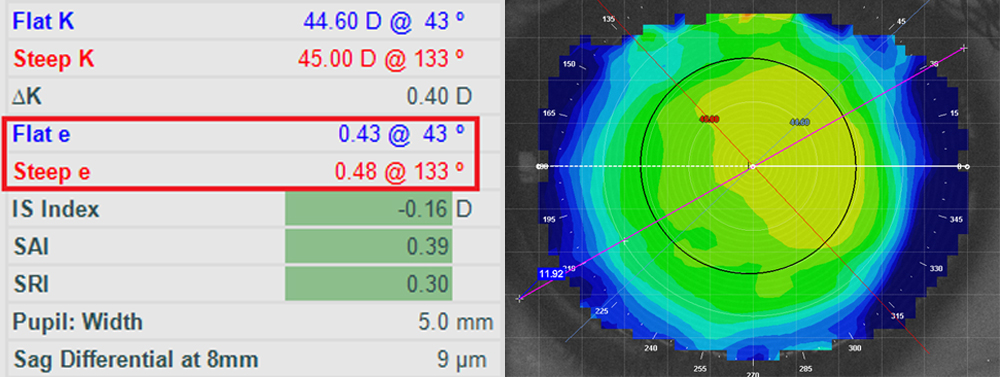
Modern topographies typically have the capability of measuring corneal eccentricity (e-value). Corneal eccentricity measures the rate of flattening from the center to the peripheral cornea. By incorporating this data into the lens design, practitioners can create lenses with improved alignment to the peripheral cornea. For example, corneas with low e-values are more spherical in shape, often requiring steeper alignment curves to create the necessary 360-degree semi-sealed alignment fit for proper corneal molding. Conversely, corneas with high e-values may require flatter alignment curves.
The horizontal visible iris diameter (HVID) can be measured more precisely using a topographer’s imaging and caliper tools compared to estimates from Pupillary Distance rulers. Unusually large or small corneal diameters may prompt practitioners to design lenses with non-standard diameters.
Figure Left: Corneal eccentricity values can help guide Ortho-K fitting. Normal corneas typically have an average e-value of 0.5, and ranges from 0.3 to 0.7. Figure Right: Iris diameters can be measured precisely using topography caliper tools.
Determine the need for a Toric Design
While some studies suggest a relatively high correlation between central corneal astigmatism and peripheral corneal elevation differences3, three topographical measurements can increase this accuracy further. Manual and automated keratometry values commonly measure the corneal astigmatism within the central 3 mm. However, Ortho-K fitting is dependent on the elevation differences of the peripheral cornea where the alignment curves land, typically at an 8 mm chord. By performing corneal topography, practitioners can more precisely determine the need for a toric design. Given the same amount of corneal astigmatism measured from keratometry, apical/centralized astigmatism may only require a spherical Ortho-K design, while corneal astigmatism that extends limbus-to-limbus may require a toric design.
Monitor refractive changes and visual complaints
Traditional gas permeable lens assessment of sodium fluorescein patterns can only provide information of the lens-cornea fitting relationship in an open-eye, seated position; this relationship can be drastically different compared to the overnight, closed-eye, supine position. Topographical maps are the best way to properly assess the true Ortho-K fitting relationship.
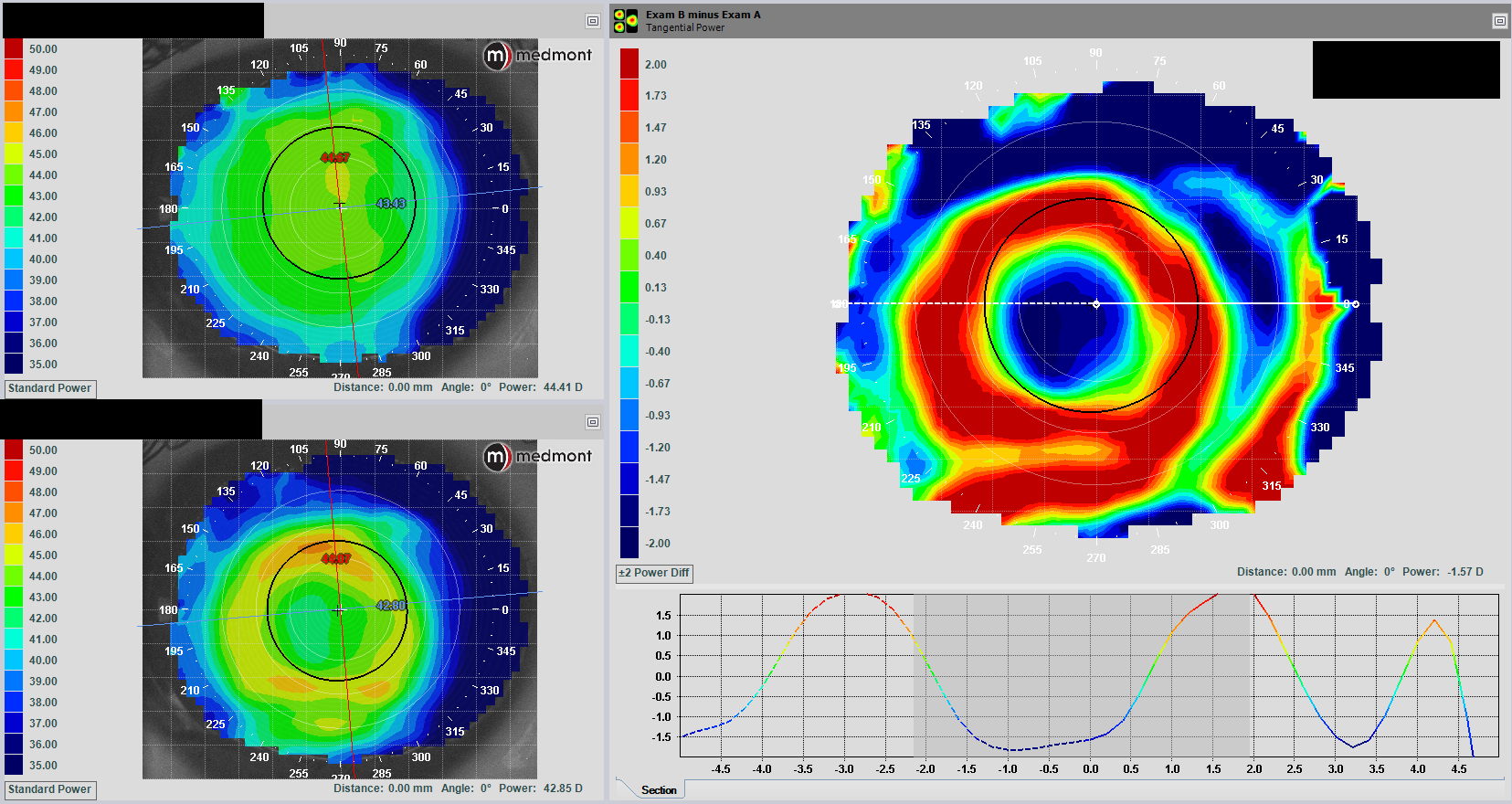
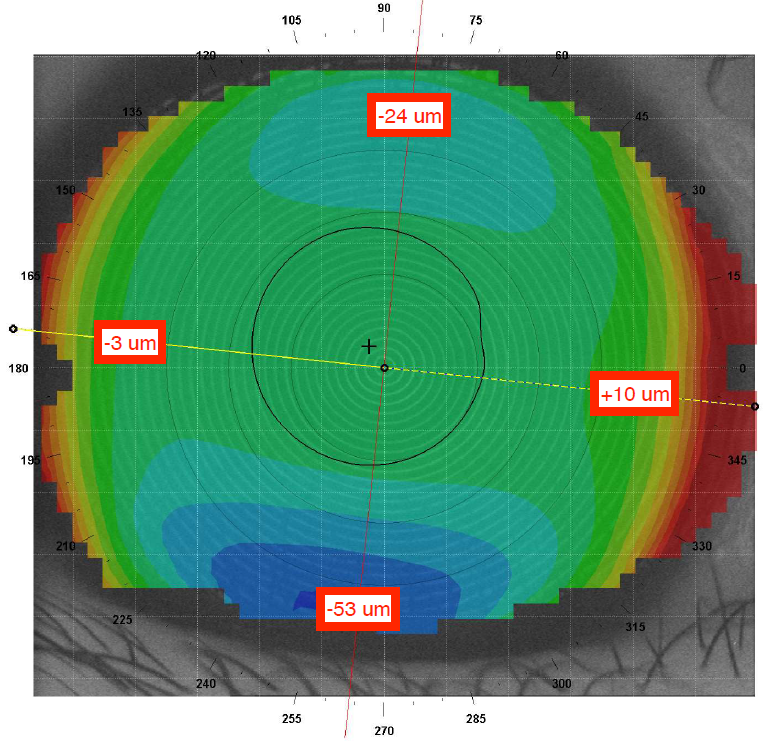
Axial maps provide refractive data such as the amount of myopic treatment produced in Ortho-K. Tangential maps, also known as instantaneous maps, provide more detailed information on the location of the treatment. Troubleshooting poor vision or symptoms of glare/halos can be difficult without topographical assessment. By analyzing these maps, practitioners can determine critical details of the Ortho-K treatment zone, including its size, quality, and centration.
Difference, or subtractive, maps calculate the difference between pre-treatment and post-treatment maps, allowing practitioners to precisely follow the location and magnitude of Ortho-K treatment. Over time, practitioners can visualize large, global changes as well as small, detailed changes on the cornea from Ortho-K.
Figure: Difference maps comparing topographies at baseline to the 1-week follow-up visit.
By understanding the benefits of corneal topography and utilizing the features of our modern instrumentation, practitioners can greatly improve the success of their Ortho-K outcomes.